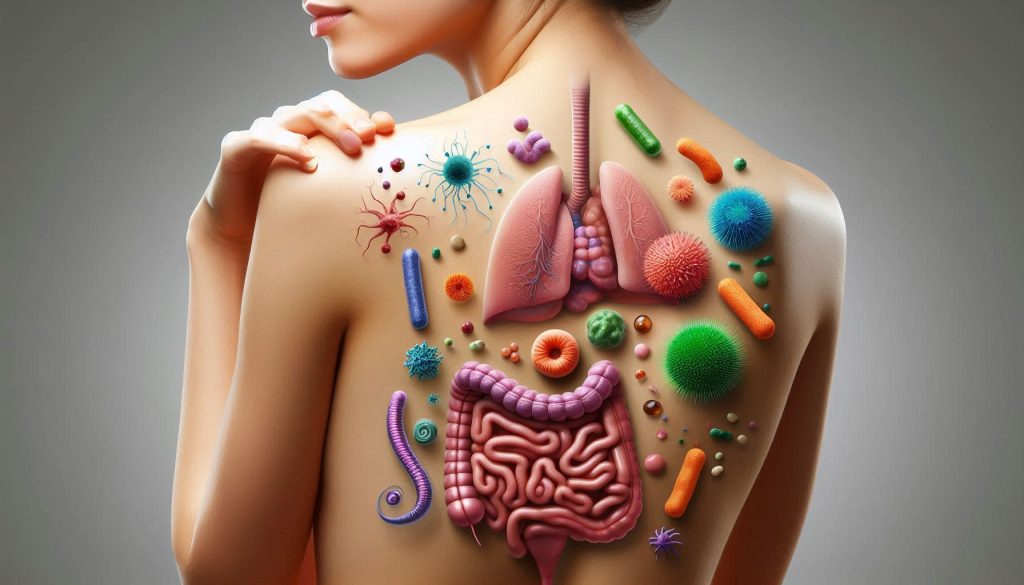
Your skin is far more than a simple covering. It’s the largest organ of the human body, weighing around 16% of your body mass, and it serves as a living, breathing interface between the external environment and your internal physiology. Beneath the visible surface lies a dynamic biological reality: your skin is home to an entire civilization of microorganisms — bacteria, fungi, viruses, and even microscopic arthropods — that together form the skin microbiome.
At the same time, deep within you, another microbial super-city thrives: the gut microbiome. For decades, scientists studied the gut primarily for its role in digestion. But over the last 20 years, research has revealed that this microbial world has a far broader influence — regulating immunity, hormones, metabolism, and even neurological processes.
What’s emerging now is a powerful realization: these two ecosystems — your gut and your skin — are intimately connected. The gut–skin axis describes a bi-directional relationship where gut microbial health can influence skin condition, and vice versa.
When the gut microbiome is balanced and healthy, it supports a smooth, clear, resilient skin barrier. But when gut dysbiosis (microbial imbalance) sets in, skin conditions ranging from acne to eczema, rosacea, and premature aging can flare.
In this extended work, we’ll journey through:
- The biology of the skin microbiome — its species, ecosystems, and roles
- The biology of the gut microbiome — its diversity, functions, and vulnerabilities
- The gut–skin axis — how communication happens through immune, metabolic, hormonal, and neural pathways
- Clinical evidence linking gut health to specific skin conditions
- Practical strategies to support both gut and skin for long-term health
- Future directions in gut–skin research and technology
The Skin Microbiome: Your External Ecosystem
The Skin as a Living Environment
Your skin is a complex, multi-layered structure with three main layers: the epidermis (outer layer), dermis (middle structural layer), and hypodermis (fatty, cushioning layer). On and within these layers live an estimated 1 trillion microorganisms.
The skin’s surface is covered by the acid mantle — a thin film made of sebum, sweat, and dead skin cells that maintains a pH of 4.5–5.5. This acidic environment discourages pathogenic growth while nurturing beneficial species.
Microbial Species of the Skin
Key players include:
- Bacteria
- Staphylococcus epidermidis — supports barrier function, produces antimicrobial peptides.
- Cutibacterium acnes — normally harmless, but can overgrow in oily conditions and contribute to acne.
- Corynebacterium species — thrive in moist environments, influence odor production.
- Fungi
- Malassezia species — lipid-dependent yeasts common in sebaceous areas; can cause dandruff and seborrheic dermatitis when imbalanced.
- Viruses
- Mostly bacteriophages that regulate bacterial populations.
- Mites
- Demodex folliculorum and Demodex brevis — live in hair follicles, typically harmless but may cause inflammation when overpopulated.
Functions of the Skin Microbiome
- Barrier Protection
Beneficial microbes compete with pathogens for nutrients and adhesion sites, preventing harmful invasion. - Immune Education
Commensal microbes “train” immune cells to tolerate harmless organisms while remaining ready to attack pathogens. - pH Maintenance
Microbes help maintain the acidic skin environment, which keeps barrier enzymes active. - Wound Healing
Some microbes produce compounds that accelerate keratinocyte migration and tissue repair.
The Gut Microbiome: Your Internal Powerhouse
Scale and Diversity
The gut microbiome is one of the densest microbial habitats on Earth. With over 100 trillion microorganisms, it outnumbers human cells and contains up to 150 times more genes than the human genome.
Major bacterial phyla include:
- Firmicutes (e.g., Lactobacillus, Clostridium)
- Bacteroidetes (e.g., Bacteroides)
- Actinobacteria (e.g., Bifidobacterium)
- Proteobacteria (various species, some pathogenic if overgrown)
Core Functions
- Digestion & Nutrient Absorption
Breaks down complex polysaccharides into short-chain fatty acids (SCFAs) like butyrate, propionate, acetate. - Immune Regulation
Gut microbes stimulate gut-associated lymphoid tissue (GALT), where 70% of immune cells reside. - Metabolic Control
Influence glucose balance, lipid metabolism, and body weight. - Neurochemical Production
Manufacture serotonin, dopamine precursors, and GABA, impacting mood and stress.
The Gut–Skin Axis: Communication Channels
Immune Pathway
Gut dysbiosis can increase intestinal permeability (“leaky gut”), allowing bacterial fragments (like lipopolysaccharides, LPS) to enter the bloodstream. This triggers systemic inflammation, which can manifest in skin redness, swelling, or chronic inflammatory disorders.
Metabolic Pathway
Gut bacteria produce SCFAs that nourish epithelial cells in both the gut and skin, strengthening barrier integrity. They also produce antioxidants and vitamins (like B-complex, K2) that benefit skin health.
Hormonal Pathway
The gut microbiome regulates hormones such as cortisol (stress), insulin (blood sugar control), and estrogens (via the estrobolome). Imbalances here can trigger acne flares or pigmentation changes.
Neural Pathway
Through the gut–brain axis, microbes influence stress perception, which directly affects skin conditions like eczema, hives, or psoriasis.
Evidence Linking Gut and Skin Health
Acne and Gut Health
- Higher prevalence of gut dysbiosis in people with acne.
- Supplementing with Lactobacillus rhamnosus GG has reduced acne severity in trials.
Eczema and Probiotics
- Infants given Bifidobacterium lactis showed reduced eczema incidence by age 2.
- Lower gut microbial diversity correlates with more severe eczema.
Rosacea and Gut Disorders
- Strong association between Helicobacter pylori infection and rosacea symptoms.
- Treating H. pylori often improves rosacea.
Psoriasis
- Gut microbiome in psoriasis patients shows reduced Faecalibacterium prausnitzii (anti-inflammatory species).
Optimizing the Gut for Better Skin
Dietary Strategies
- Prebiotics: Onions, garlic, asparagus, leeks, chicory root.
- Probiotics: Yogurt, kefir, sauerkraut, kimchi.
- Polyphenols: Green tea, berries, cocoa.
- Omega-3s: Salmon, flaxseed, walnuts.
Lifestyle Factors
- Stress Management: Meditation, yoga, deep breathing.
- Adequate Sleep: 7–9 hours to reduce cortisol spikes.
- Hydration: 2–3 liters daily for optimal circulation.
Supporting the Skin Microbiome
- Use pH-balanced cleansers.
- Avoid over-exfoliation.
- Moisturize with products containing ceramides or natural oils.
- Limit antibacterial soaps to hands only when necessary.
The Future of Gut–Skin Science
- Microbiome-targeted skincare with live probiotics.
- Personalized diet plans based on stool analysis.
- Postbiotic creams delivering beneficial microbial metabolites to skin cells.
- Fecal microbiota transplants (FMT) for severe inflammatory skin diseases.
Conclusion
Radiant, healthy skin isn’t the result of the latest cream or serum—it begins deep within your digestive system, where trillions of beneficial microbes form your gut microbiome. These microscopic allies play a vital role in regulating immunity, managing inflammation, and supporting metabolic balance, all of which directly influence your skin’s clarity, tone, and resilience.
When your gut is in balance, it sends positive signals to your skin, helping reduce irritation, prevent breakouts, and maintain a youthful glow. Conversely, gut imbalances can trigger inflammation, leading to issues such as acne, eczema, dryness, or premature aging.
Achieving harmony between your gut and skin requires a holistic approach: nourishing your microbiome with fiber-rich whole foods, probiotics, and prebiotics; managing stress through mindfulness and rest; and complementing internal care with gentle, supportive skincare.
When these elements work together, your skin reflects your internal well-being—radiating vitality, strength, and beauty that no cosmetic product alone can replicate. True skin health begins from the inside out, with a thriving gut as the foundation for a vibrant, confident you.
SOURCES
Bowe, W. P., & Logan, A. C. (2011). Acne vulgaris, probiotics and the gut–brain–skin axis—Back to the future? Gut Pathogens, 3(1), 1–11.
Byrd, A. L., Belkaid, Y., & Segre, J. A. (2018). The human skin microbiome. Nature Reviews Microbiology, 16(3), 143–155.
Chen, Y. E., Fischbach, M. A., & Belkaid, Y. (2018). Skin microbiota–host interactions. Nature, 553(7689), 427–436.
Egert, M., Simmering, R., & Riedel, C. U. (2017). The association of the skin microbiota with health, immunity, and disease. Clinical Pharmacology & Therapeutics, 102(1), 62–69.
Findley, K., & Grice, E. A. (2014). The skin microbiome: A focus on pathogens and their association with skin disease. PLoS Pathogens, 10(11), e1004436.
Gallo, R. L., & Nakatsuji, T. (2011). Microbial symbiosis with the innate immune defense system of the skin. Journal of Investigative Dermatology, 131(10), 1974–1980.
Gupta, V. K., Paul, S., & Dutta, C. (2017). Geography, ethnicity or subsistence-specific variations in human microbiome composition and diversity. Frontiers in Microbiology, 8, 1162.
Hooper, L. V., Littman, D. R., & Macpherson, A. J. (2012). Interactions between the microbiota and the immune system. Science, 336(6086), 1268–1273.
Kober, M. M., & Bowe, W. P. (2015). The effect of probiotics on immune regulation, acne, and photoaging. International Journal of Women’s Dermatology, 1(2), 85–89.
O’Neill, C. A., Monteleone, G., McLaughlin, J. T., & Paus, R. (2016). The gut–skin axis in health and disease: A paradigm with therapeutic implications. BioEssays, 38(11), 1167–1176.
Petersen, C., & Round, J. L. (2014). Defining dysbiosis and its influence on host immunity and disease. Cell Microbiology, 16(7), 1024–1033.
Rinninella, E., Raoul, P., Cintoni, M., Franceschi, F., Miggiano, G. A., Gasbarrini, A., & Mele, M. C. (2019). What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms, 7(1), 14.
Salem, I., Ramser, A., Isham, N., & Ghannoum, M. A. (2018). The gut microbiome as a major regulator of the gut–skin axis. Frontiers in Microbiology, 9, 1459.
Sanford, J. A., & Gallo, R. L. (2013). Functions of the skin microbiota in health and disease. Seminars in Immunology, 25(5), 370–377.
Williams, M. R., & Gallo, R. L. (2017). The role of the skin microbiome in atopic dermatitis. Current Allergy and Asthma Reports, 17(11), 90.
Zheng, D., Liwinski, T., & Elinav, E. (2020). Interaction between microbiota and immunity in health and disease. Cell Research, 30(6), 492–506.
HISTORY
Current Version
Aug 8, 2025
Written By:
SUMMIYAH MAHMOOD